Webinar broadcast: youtube.com/gyncare
Presenter. Michal Michna
gynaecologist from the Gyncare centre in Košice
Watch the webinar. You will learn about the causes of age-related reduced fertility and, at the same time, the options for addressing them. It is important to point out that postponing pregnancy plans to an older age is associated not only with a reduced chance of spontaneous pregnancy but also with an increased risk of early pregnancy loss and pregnancy complications.

It is important for every woman to have enough complete and objective information about fertility and to consider it when planning her pregnancy. We often receive negative information related to the fact that pregnancy at an older age is risky. The fact that women are pushing back the age of pregnancy and childbirth to an older age is also heard in the media. However, there is a lack of real information on how fertility actually is. Where are the limits of female fertility? All of us know that a 70-year-old woman is no longer fertile. There are various inaccuracies about the fertile (childbearing) age or the median fertile age and the unrealistic expectations associated with them. We don’t want to scare you with the facts about female fertility, but to help you make the right decisions in time.
To the question, “At what age is a woman too old to be pregnant?” European countries were answered by a difference of up to one decade. Despite being socially, culturally and socially close to each other, the age of 37 to 45 was given in their answers. The results show that in some countries a woman is considered too old to become pregnant at 45. In some places, they already think this of much younger women. Society’s views are very individual. Increasingly, there are bombastic reports in the media that well-known women have become pregnant or given birth at an older age, in their fifties. However, these sensations are just the tip of the iceberg. The celebrities in the media reports are exactly the same women as the other ones. They may have greater financial means, but their fertility is exactly the same. We don’t know their full story, which means their journey to having a baby could have been complicated and full of setbacks. There is no mention of how they got to their desired destination either. The vast majority of pregnancies and births around a woman’s fiftieth birthday are achieved thanks to eggs that are significantly younger than the pregnant woman. Often these are eggs from the donor, or eggs that the woman has had frozen for a decade, and perhaps even before she became pregnant.
When we talk about older age, in the case of female fertility we consider it to be already above 35 years of age. The global trend is clear. Pregnancy shifts to an older age, when it is more difficult to become pregnant and to end the pregnancy by giving birth to a healthy fetus.
Women’s age is a fundamental and key factor that influences their fertility and reproductive outcomes. Despite the fact that many women in their forties still have regular cycles and their baseline hormonal profile does not indicate a major problem, we still say that they are functionally infertile and their chances of achieving pregnancy are slim to none.
How many women are affected? In 2004, she gave birth after 35. year of life, around 4 000 women. Data from 2020 show an increase to 10 000 women, which is a truly enormous increase. We assume that the number of women trying to conceive at this age is much higher. Their chances are already low, and therefore many women do not even make it into the birth statistics.
Spontaneous fertility in women is at a younger age, up to 30. year of life, approximately the same. In healthy couples, the chances of conception are around 25% per cycle and then decrease. After the age of 35, the decline in fertility is enormous. The chances of women after 40 are very low indeed, about one per cent, even if they have a healthy partner. Why is this so?
One reason is the decreasing chances of spontaneous conception. When a woman’s fertility declines spontaneously, the risk that a pregnancy will end in spontaneous abortion naturally rises. The risk of pregnancy loss at a young age is relatively low. By the age of 30, it is approximately up to 10%. After the age of 40, up to a third of pregnancies can end in failure , and after the age of 45, it is almost half.
Effect of egg quality on a woman’s fertility
The quality of eggs has a major impact on fertility, which changes significantly as a woman ages. While men form new sperm constante throughout life, women are born with a finite supply of eggs that is constantly dwindling. The eggs disappear by a natural process that may be faster in some women, slower in others. Although women have one to two million eggs at birth, only about four hundred eggs mature and are released at ovulation during fertile life. All others will cease to exist. What is essential is the actual real egg quantity and the real ovarian reserve. In an artificial insemination cycle, a reduced egg reserve causes a much smaller number of eggs that we are able to retrieve to be ready for ovulation in a given cycle. When the number of eggs drops below a critical value, a woman enters menopause, menstruation disappears and there is a significant drop in hormones. Despite the fact that even during menopause, she has some amount of eggs at her disposal, today’s medicine and science no longer have the means to obtain these eggs.
Influence of external factors on egg quality
The decline in eggs is constant, continuous and we cannot fundamentally influence it in a positive direction. The ovarian reserve can be adversely affected by external factors, including ovarian surgery, endometriosis, endometriosis surgery, or the external effects of chemotherapy and radiotherapy, which can significantly reduce both the number and quality of eggs. There are women who have a genetic predisposition to premature menopause and their ovarian reserve declines much more markedly and more rapidly. External influences, such as smoking, cause an earlier onset of menopause and reduce the functional potential of the ovary.
Ovarian reserve tests
Ovarian reserve tests are available to all women through a network of outpatient gynecologists. This is an AMH (Anti-Müllerian Hormone) test and an examination of the number of tiny follicles in the ovary that are present during the current cycle. On the basis of these examinations we can determine the potential of the real ovarian reserve in a given woman.
Egg quality
Another crucial factor is the quality of the eggs. A healthy egg contains 23 chromosomes. If it fuses with a healthy sperm, which also contains 23 chromosomes, it is likely to produce a healthy embryo. Unfortunately, the number of genetically unhealthy embryos, which we call aneuploid emb ryos, increases with age in women. Over the age of 43, the vast majority of eggs are aneuploid. The underlying problem of why these women fail to conceive is not the quantity and quality of hormones. This happens because the quality of their eggs, and thus the quality of the embryos, is already very low. We cannot individually test and evaluate the quality of the egg. The only evaluable criterion for assessing the quality of the egg is the pregnancy terminated by delivery. Nowadays, however, we have the possibility to genetically examine embryos.During an artificial insemination cycle, we sometimes detect an increased number of genetically bad (aneuploid) embryos even in healthy women at a young age. They may also have 20%-30% aneuploid embryos. However, there is a standard increase in poor embryo quality, especially after the age of 40, when on average only two out of ten embryos have the correct number of chromosomes.
It is of course individual, but these statistics complete the overall picture. Egg quality is a crucial factor that affects a woman’s fertility.
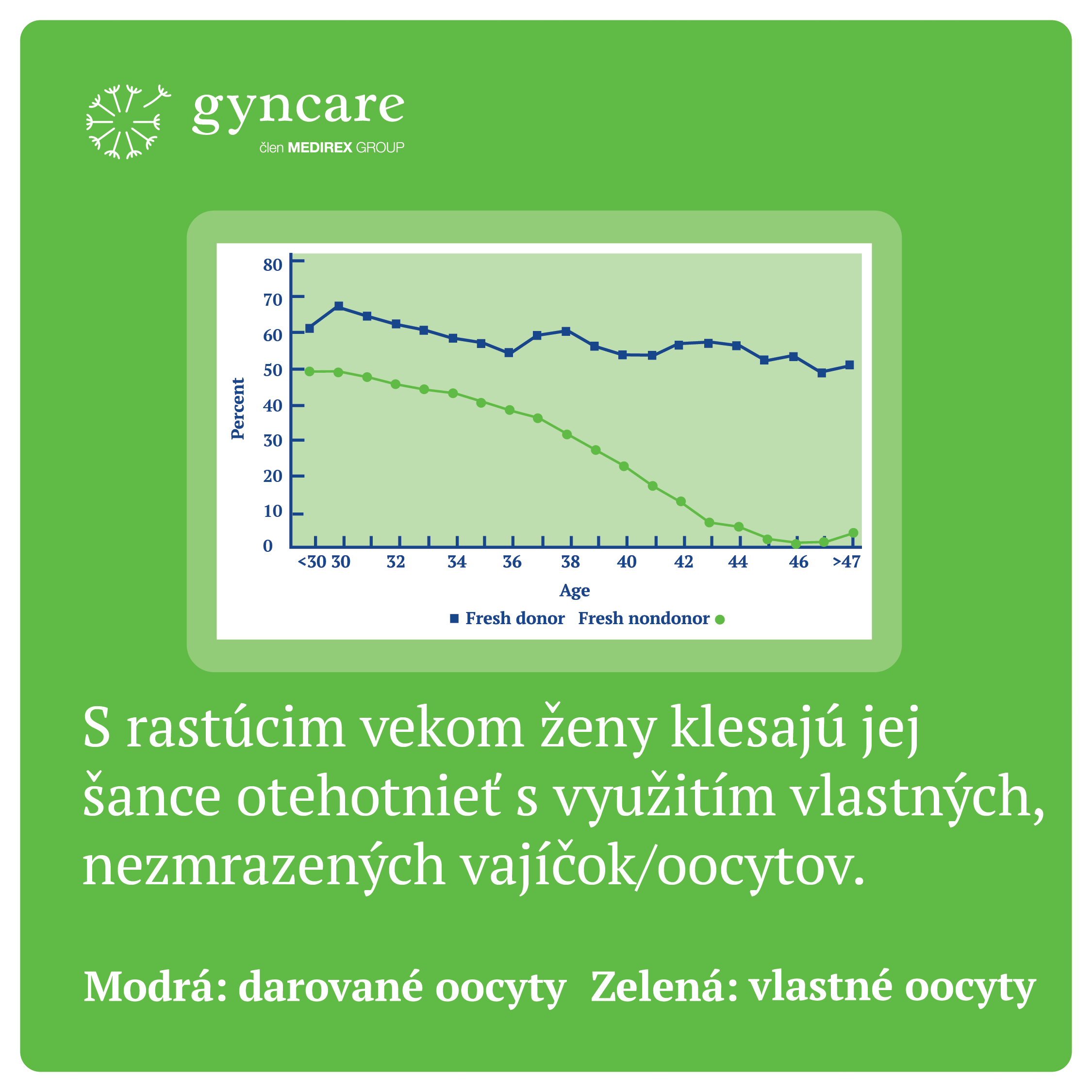
If we look at the graph showing the percentage of pregnancies after fresh embryo transfer, we can see in the green curve that the success rate of deposits (transfers) of own eggs (oocytes) is about the same up to the age of 30 and varies between 40-50%. By 35. There is a gradual decline after the age of 35 and a very steep decline after the age of 35. The chances of getting pregnant using one’s own eggs over the age of 40 are really low, only about 1%. The blue curve represents the success rate of embryo transfers that have been made from eggs obtained from a donor who is healthy and young. We can see that the curve of successful transfers of such embryos does not fall substantially even in women who are 40-45 years old. This implies that the quality of the egg is the primary determinant of deposit success.
The risk of endometriosis and uterine fibroids can negatively affect fertility in some cases, and their incidence also increases with age.
Is it possible to increase the quality of eggs?
Currently, there is no treatment procedure by which we can increase the quality of eggs. In the same way, we can not increase the real ovarian reserve. An option to preserve fertility is to freeze an adequate number of eggs at a younger age when we expect them to be of higher quality. This also protects the eggs from future possible negative factors that can significantly reduce their quality. For example, in cases where the patient is facing chemotherapy, pelvic radiotherapy or major surgery that will affect the ovaries. We cannot increase fertility by changing lifestyle, but we can prevent fertility from declining significantly by making positive lifestyle changes. Significant fertility decline is mainly caused by smoking, obesity and metabolic syndromes. Every individual and couple has individual reproductive potential. Even women in their 30s may have significantly reduced egg quality or quantity and may suffer from premature menopause. On the contrary, some women, even after forty, get pregnant very easily and have no problem carrying a child. There is no guarantee what course the fertility decline will take – whether it will be smooth or steep.
Examples from practice
Example 1
The first case report concerns a 39-year-old female patient who has a history of pregnancy loss that occurred when she was 25 years old. She had been trying to get pregnant for 7 years. We found a high proportion of abnormally shaped sperm in her partner. The patient’s ovarian reserve was adequate (AMH 2.4 ug/l). The couple opted for infertility treatment with the IVF ICSI method. Nine days of hormonal stimulation began, during which seven follicles grew, from which we retrieved six eggs and all were fertilized. At the end of culture after five to six days, we obtained three embryos. Two embryos were frozen and one embryo was inserted into the uterus by fresh transfer. The transfer resulted in pregnancy. Although the statistics sometimes look unfavourable, they do not apply to everyone.
Example 2
As another example, consider the case of a 39-year-old woman who already had one child. Her partner had a very severe spermiogram disorder at the current period – few sperm, which were also moving more slowly. The couple was fully examined and no major cause of infertility was found apart from the male factor. The woman had already undergone two unsuccessful IVF cycles in the past and at 39 years of age had an ovarian reserve quite adequate for her age. She entered the third cycle. After stimulation, we obtained eight eggs, six of which fertilized. Subsequently, a fresh embryo transfer was performed, which was unsuccessful. Surprisingly, despite their advanced age, several embryos were cultured and cryopreserved (frozen). All cryopreservations were successful. After a failed fresh transfer, she entered her fourth cycle of stimulation with low doses of hormones. We obtained two more oocytes. All the embryos obtained were transferred in turn, but we did not achieve pregnancy. During the fifth cycle, which was at the age of 41 years of the patient’s life, two oocytes were retrieved. We obtained two embryos from them, which were transferred on the fourth day. This fifth IVF resulted in a pregnancy. This example shows that egg quality is individual and can change from one egg to the next.
Male fertility is not an often discussed topic, either among the general public or in the media. We have long thought that male fertility does not change, but the opposite is true. The higher age of men also affects the chances of conception and has an impact on the health of the fetus, but also on the health of the offspring. However, the decline in fertility in men occurs much later, that is, between 40. – 50. year of life. After the age of 50, there is a decline and deterioration of the spermiogram. It is generally known that pregnancies of older women are at greater risk of Down syndrome. The same is true for men, but the risk in this case is not as high as for women. As men get older (after 40-50 years of age), the risk of some pregnancy complications increases, as does the risk of spontaneous miscarriage, premature birth, some neuropsychiatric diseases, and the risk of oncohematological diseases in the offspring. Male fertility is also gradually declining, but the decline is not as rapid and extreme as for women.
Pregnancies at an older age are risky, but our job is not to scare you about it. It is important to inform about this, but above all about the options we can use to reduce this risk of potential complications. The cause of pregnancy complications is not only age, but often also diseases such as high blood pressure, overweight, diabetes or cardiovascular disease. At older ages, the risk of pre-eclampsia, which is high blood pressure in pregnancy that is associated with dysfunction of certain organ systems, increases. Then there is the risk of gestational diabetes, preterm birth, multiple pregnancies and some chromosomal abnormalities such as Down syndrome. The risk of genetic disorders rises significantly after 35. year of life and in 40. year of life, the ratio is about 1:100. The risk of non-chromosomal, morphological or structural disorders is also more or less the same due to increasing age. With this information, we want to draw attention to prevention. If we have a medical history or other reason to examine the embryos preimplantation, we can do so during the IVF cycle. This allows us to find out the basic composition of the chromosomes and gives us the opportunity to select from several embryos the one that has the best chance of achieving pregnancy, and the best chance of such a pregnancy being healthy.
Pre-implantation genetic diagnosis is not automatically indicated for every couple, but many may benefit from this embryo screening. For example, in cases where several embryos are available, in older women, after repeated unsuccessful embryo transfers, in cases where pregnancy loss of the foetus was caused by a chromosomal disorder , or the partners had a child with such a disorder, and after treatment for oncological diseases that put the offspring at risk of chromosomal disorders. For the purpose of pre-implantation genetic diagnosis, we take a small amount of cells from the future placenta from a five-day-old embryo, which will not be missing. Thanks to this, we can find out whether a given embryo is genetically healthy and, above all, we have the opportunity to select the best quality embryo with the best potential for a healthy pregnancy from a number of embryos.
By screening during pregnancy, it is possible to capture and examine circulating fetal DNA in the mother’s blood. These are non-invasive prenatal tests – NIPT, which include the TRISOMY test. Due to its high sensitivity, the TRISOMY test can exclude the inaccuracies of other tests, such as the triple test, and thus reduce parental concerns about fetal health.
Pregnancy complications associated with a woman’s advanced age
Pre-eclampsia, premature birth, as well as gestational diabetes are often referred to as pregnancy complications associated with older age. The risk of gestational diabetes increases with increasing age. In this case, there is also the possibility to undergo a screening test to detect this risk. Thanks to this, you can intervene preventively and adjust your weight and lifestyle before conception, and thus significantly reduce the risk of developing gestational diabetes. Good cardiovascular health and good fitness significantly reduce the risk of heart disease and the risk of premature birth. If we detect risks leading to preterm birth in advance, for example by measuring the cervix, we can intervene preventively, for example by administering progesterone.
Pre-eclampsia is a very common condition, occurring on average in 8% of women. The incidence of this disease also increases at older ages. It is associated with high pressure, impaired kidney function or certain organ systems. Between 11. a 14. week, we can intervene in at-risk patients and administer aspirin as a preventive measure to reduce the risk.
What if, despite your advanced age, you long for a child?
We understand that wanting a baby is unavoidable and often doesn’t take your age into account. First of all, it is important to assess whether pregnancy is safe for you. Adjust any poor health, adjust pressure treatment with adequate medication, optimize weight, fitness and lifestyle, and to compensate for illnesses if you have been diagnosed. In this way, you reduce the risk of pregnancy complications.
Your chances of getting pregnant and carrying a healthy foetus should be discussed with a reproductive doctor who will assess your options and risks.
When is it realistic to have expectations of a successful pregnancy with your own eggs and when is it time to look for other options, such as an IVF cycle with donated eggs? In order to assess this, it is important to know your ovarian reserve and health status.
We know that even modern assisted reproduction methods cannot compensate for age-related fertility loss. It will probably be a few more decades before we repeat this sentence to you: the success rate of IVF cycles decreases with increasing age. That said, if you’re having trouble getting pregnant or even a recommendation from your doctor to go to IVF, don’t wait another 2, 3, 4 years. At older ages, infertility treatment can be even more complicated. Pregnancy at an older age is really specific and requires care to be as thorough as possible and using the most up-to-date diagnostic methods.
Your chances of getting pregnant and carrying a healthy foetus should be discussed with a reproductive doctor who will assess your options and risks.
Questions
Is it possible to influence the quality of oocytes by an appropriately chosen stimulation method?
Yes, it is probably possible, but we cannot assess the quality of the oocytes or their maturity before stimulation. If we change the type of stimulation, i.e. the type of protocol, we can only evaluate this on the basis of the result, to which we can react adequately and decide how to proceed.
If you have been trying to conceive for a long time and there are known medical issues that cause infertility in couples, you really need to choose a treatment that addresses this infertility. Even with a severe spermiogram, the chances drop significantly. They are never zero, but if infertility has been going on for several years and multiple factors are present, then the recommendation to go for IVF is adequate.
How can egg quality be improved around the age of forty?
If we do not take into account experimental possibilities, we cannot substantially increase the quality of the eggs. However, as long as a woman has a good ovarian reserve, there is a chance that some of the eggs will be of good quality and pregnancy will be achieved.
I’ll start from the end, a lot of pregnancies end in miscarriage, yes. It is not definite, some women who miscarry may be healthy and young. This is an accidentally occurring error in the fusion of two cells, the sperm and the egg. It is a normal part of human reproduction. Much of abortion is not our fault and we cannot control it. Yes, women with PCOS can get pregnant, and PCOS is a diagnosis of relative infertility, meaning that someone can succeed. As for other diagnoses and special examinations. There are couples who do not need special tests, for example, a pathological spermiogram – we cannot resolve this in any other way than with the IVF ICSI treatment method. As long as the woman is healthy, there is no need to examine her fundamentally. If there are failures along the way to pregnancy, this points to the possibility of other causes and more complex and extensive investigations are recommended. My point is that not everyone needs all the scans. They may be suitable for someone, for someone not. However, it must be said that every doctor has his own opinion. As long as she communicates properly why she recommends the examination, then it’s always about a discussion between the doctor and the couple. If someone recommends genetic testing and communicates it properly, that’s up to you. You can undergo it or not.
If you’re 31 and not planning to get pregnant yet, that’s really an adequate age to freeze your eggs, that’s the right decision. None of us can assess your fertility. What the odds are, I would probably only guess. Uterine fibroids can cause pain, can affect reduced fertility and sometimes it is difficult to prevent further fibroid growth. The most appropriate thing is not to postpone pregnancy far into the future. Although fibroids do affect fertility, this problem can be addressed, unlike egg quality, which cannot be solved at an older age.
The crucial question is whether the couple is trying to get pregnant. If a man has his spermogram examined for some reason and it is abnormal in some parameter, such a spermogram may or may not indicate reduced fertility. We can only determine this when fertility is realistically reduced. If an unsuccessful attempt at conception has been going on for some time, it can be assessed that the spermogram in question does not lead to pregnancy. At the moment, we don’t know of a magic pill that can fix it. If there is an abnormal spermogram, it is always possible to consult a urologist. He is a doctor who specializes in male fertility and sexual health and to rule out any medical problem of the male genital tract.
It is very likely that donated eggs can contribute very significantly to a successful pregnancy.
Low AMH values do not automatically mean infertility. If the woman is young and healthy and has a patent fallopian tube and the partner has a good spermogram, then low AMH may not be a significant problem if you are trying to conceive at that particular time. But it may pose a significant problem in the later future. If the AMH values are low and the couple has been unsuccessfully trying for pregnancy for some time, then it is advisable to recommend a method of infertility treatment – IVF. Low AMH values may not be a major problem in the case of a young woman, because with a small number of eggs there is a good chance that they will be of good quality, and therefore good quality embryos. Conversely, in women of advanced age, very low AMH values mean an extremely small number of eggs, very low chances, whether in spontaneous or artificial insemination, since it is assumed that those few eggs are already of reduced quality.
If you couldn’t get pregnant spontaneously, then yes. The IVF method is an appropriate treatment for infertility if you have antibodies that are directed against sperm.
In the case of elevated NK cells, intralipid infusions are one option to attempt successful embryo fertilization. Especially in cases where the woman has already undergone unsuccessful embryo transfers.
Untreated hypothyroidism has a major impact on a healthy pregnancy. Reduced thyroid function can lead to a baby not being born healthy. In these cases, compensation for reduced thyroid function is important.
What protocol would you choose for a woman over the age of 40? Long, short, combined?
First of all, it depends on the ovarian reserve. I would decide based on what protocol you have done in the past and with what results. Individual assessment of the patient is important, there is no general prescription.
If you don’t have frozen eggs yet and you know that you don’t plan to be pregnant anytime soon, then the decision to freeze your eggs is definitely the right one. Ideally this will be with adequate ovarian reserve. However, it should be noted that the chances of obtaining a suitable egg are already reduced at this age, because the lower quality of the eggs, even with their greater number, reduces the success of the whole process. However, it is certainly better to decide to do so now rather than later. Because the risk of failure increases even more as time goes on.
I am 25 years old, my husband is 29 years old and he was found to have oligoteratozoospermia. She has 0% morphology and we have been trying for a baby for a year. We were recommended IVF treatment for infertility. Is there any chance of success with the IUI method? What are the chances of it working the first time? I’m very afraid of that morphology.
If we have a spermiogram that is significantly abnormal in several or one of the parameters, the chances of achieving pregnancy at insemination are extremely low. It is a method that makes no sense to use in this case. The recommendation of artificial insemination, i.e. IVF cycle, is adequate in this case.
PSOS syndrome is often associated with overweight or obesity. The first step of treatment in such a case is weight correction. However, this does not apply to everyone. Some women have anovulation despite having a normal weight. There is no miracle cure for this syndrome. For example, preparations containing myoinositol are recommended.
Is it advisable to have reproductive immunology before IVF?
If there is a known factor causing the infertility problem, for example, if you have an obstructed fallopian tube, then undergoing reproductive immunology testing is not fully justified and is not recommended by the world’s professional societies in this case. If it is a couple that has already had unsuccessful IVF, or immunopathology has been detected and testing has been indicated by an immunologist, then this is certainly an appropriate step.
What is your experience with the success rate of pregnancy in endometriosis?
Our experience is that there are cases where women get pregnant without any problems to cases where the ovaries are unfortunately in a state that the chances are very low, whether it is spontaneous conception or thanks to IVF. This is a whole spectrum of individual cases.
Up to what age is it appropriate to freeze eggs? Can an egg from a woman in her 40s be frozen?
It is possible, but at this age there is already a higher risk of aneuploid embryos. It’s always up to the woman to decide, who is educated about the options and about the chances.
The quality of embryos is determined primarily by age. The chance of a euploid embryo is greatly reduced. It’s more about the repetition of the whole process, thereby accumulating chances of success, not the type of protocol.
If the woman was of an older age when the IVF cycle was performed, the use of donated sperm will not resolve the quality of the egg. It may solve the problem if there is presumed poor quality or inadequacy of the sperm, but it will not solve the egg quality problem. A suitable alternative may be to use donated eggs.
At 39 years of age and five years of trying to conceive spontaneously, an IVF cycle is clearly indicated. If the thyroid gland is well controlled with medications that replace its function, then it is not a problem that causes infertility. The period of infertility is indicative of a different problem. Moreover, the chances decrease with increasing age, and very steeply. Metformin is not used in thyroid cases. In Slovakia, IVF is partially covered only up to 40. year of life, i.e. the financial cost of treatment rises later. We definitely recommend not to delay IVF treatment any longer.
How long after unsuccessful IVF is it appropriate to try again?
As long as the woman is young and there are no factors that have been found to be significantly aggravated by waiting, the couple can take a break. Conversely, if a woman is 39-40 years old, waiting can significantly reduce the chances of success.
At 1% spermiogram and at a given age, professional societies recommend an IVF cycle. You can undergo IUI, but the chances of success are reduced if there is only one percent of normal sperm.
The chances are very slim indeed. At such values we cannot count on stimulation, at the end of which an adequate number of eggs will be obtained. Higher chances are achieved when using donated eggs. As for waiting for a donor, our coordinators will give you all the information you need. You can make an appointment with us for a consultation and discuss the details.